A patient was admitted to the hospital for repeated exacerbations of COPD, which had been lasting for several weeks. Chest pain appeared in the morning of the day of admission. Significant elevation of troponin level was revealed at emergency. ECG showed no pathology. Acute coronarography was performed. Tandem stenoses were found in right coronary artery. Three drug-eluting stents were implanted. Hypotension around 60/40 mmHg appeared during the intervention. No symptoms did accompany it. The patient was admitted to ICU. Lab tests revealed CRP 100 mg/l, no leucocytosis and procalcitonin 0.41 ng/l.
The patient further admitted that he had suffered from shivering in the morning. He did not measure his body temperature. Quick immunochemical screening test with the use of nasopharyngeal smear was negative for influenza A and B. The patient presented with spasticity; however, his breathing did not worsen. Hypotension 90/40 mmHg without the necessity of administration of catecholamines, sinus rhythm, 60 bpm, sufficient SpO2 with nasal cannula 2 l/min.
What caused the hypotension? Was the aetiology cardiac, hypovolemic or septic (potential infection)?
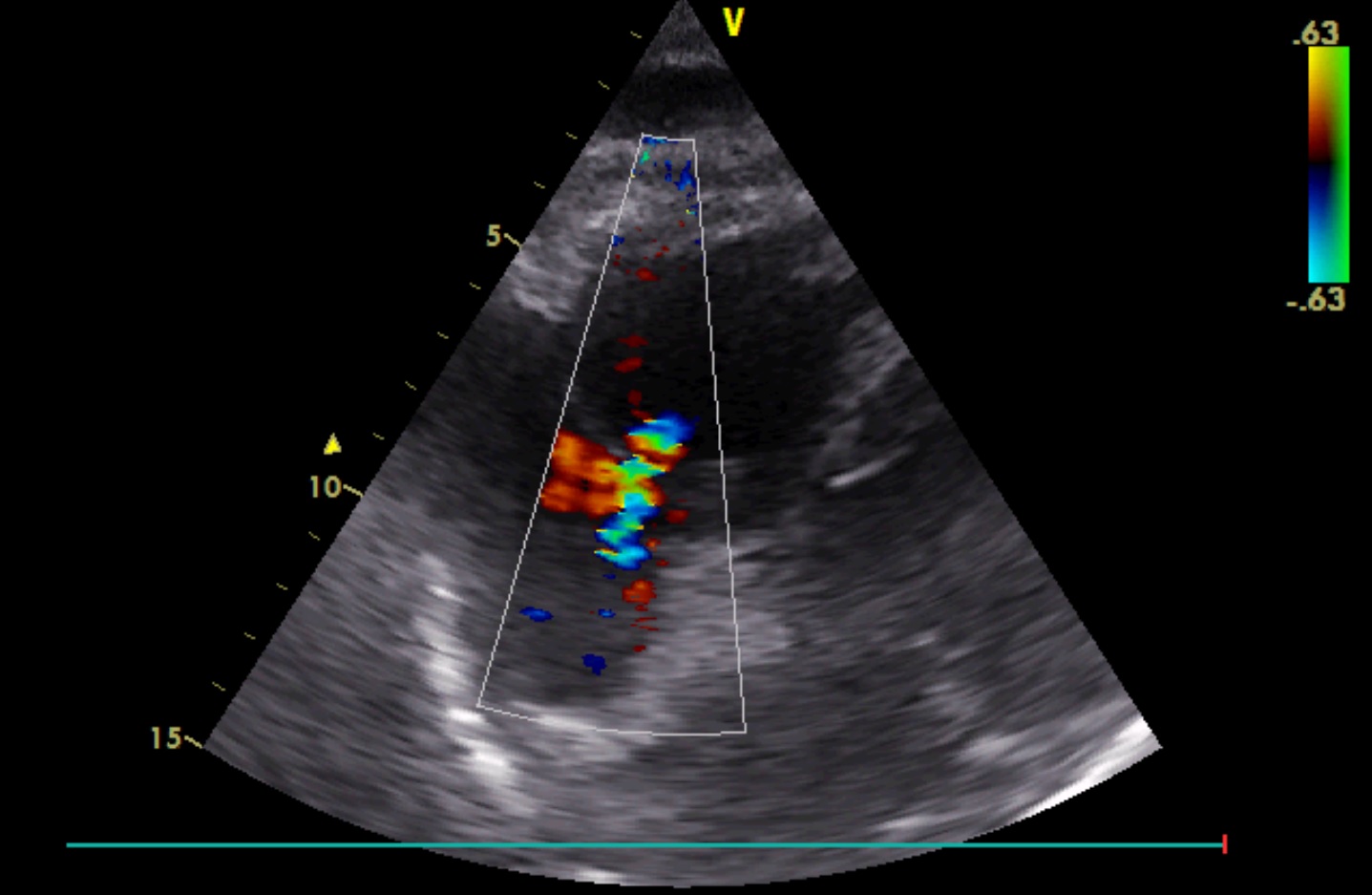
We performed ultrasonography. We started the examination with echocardiography to exclude cardiac insufficiency and tamponade, considering almost complete obturation of the right coronary artery:
<h3>