An 88-year-old patient was admitted to the ICU for decompensation of COPD and hypercapnia. Orotracheal intubation was necessary due to unconsciousness.
The patient was extubated two days later. Inflammatory markers were not elevated. Severe tachypnea (up to 60/min) persisted on day two after extubating. The patient was hypoxemic even though he received oxygen (6 l/min via face mask), without the tendency of retention of CO2. Auscultation revealed silent breathing sounds with prolonged expiration, weakened breath sounds basally bilaterally and crackles ventrally. The patient did not show signs of the mucus presence – she did not tend to cough out. Central cyanosis appeared quickly when the oxygen mask was removed. Haemodynamics was stable with atrial fibrillation 100/min, blood pressure 140/80 mmHg (invasive measurement), good peripheral perfusion and without any oedema.
Chest X-ray:
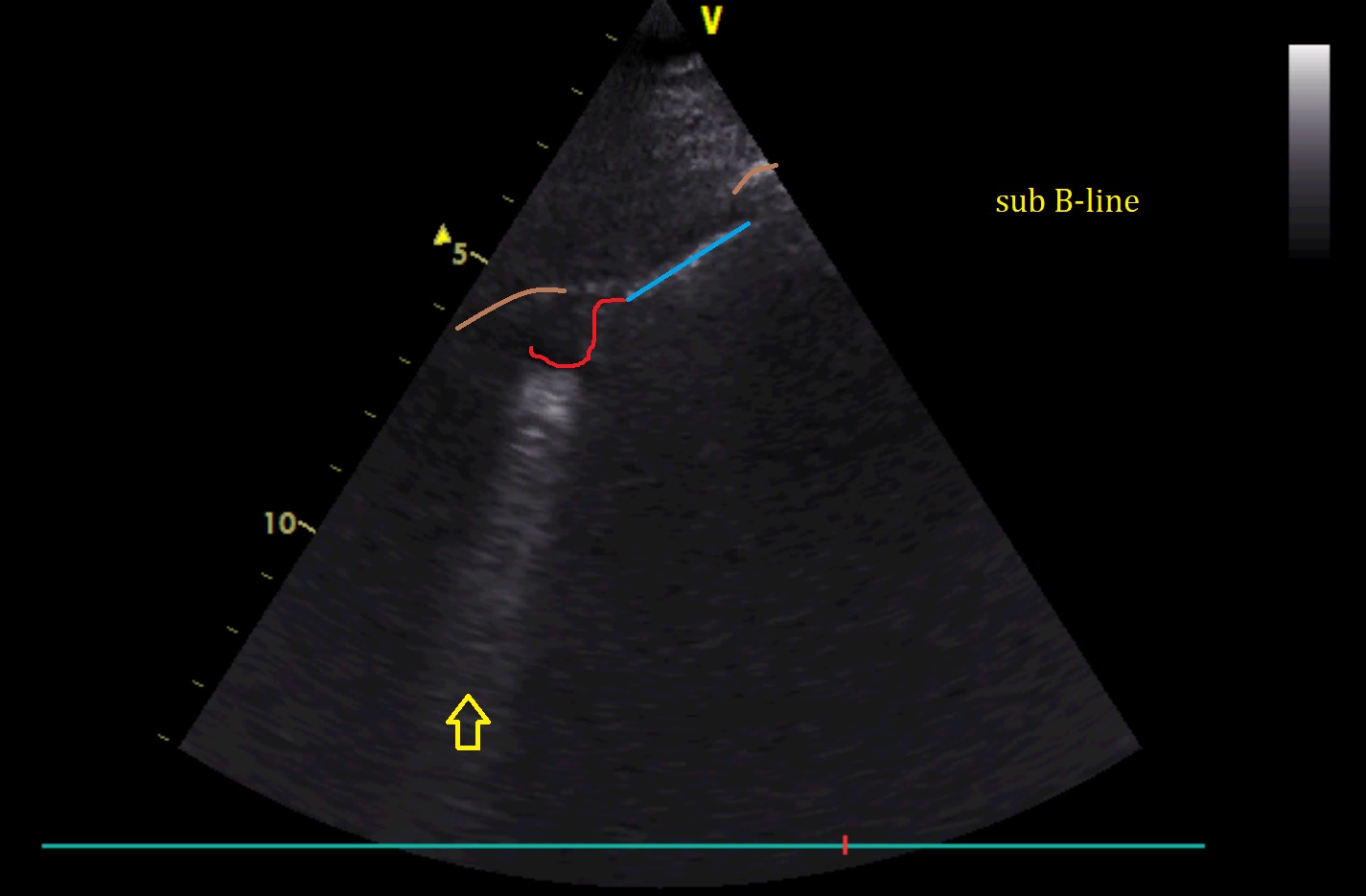
Lung ultrasonography: