An 82-year-old patient underwent surgery for big retrosternal goitre. The jugular approach was used. Patient´s medical history had been minimal so far. Bleeding into surgical wound occurred shortly after surgery. Prompt re-intubation and surgical revision were necessary. A short period of haemodynamic instability occurred during surgical revision. Blood loss of 500 ml was compensated via administration of the crystalloid solution. The patient was admitted to our ICU with noradrenalin 1.5 mg/hour (approximately 0.35 ug/kg/min). Haemodynamics stabilised after recovery from anaesthesia and supplementation of blood loss via administration of the crystalloid solution.
No bleeding was present on day 2. The patient was extubated without any problem. Antihypertensive drugs had to be administered due to hypertension. The patient did not present with any symptoms. However, it was difficult to withdraw oxygen support even though physical examination did not reveal any pulmonary pathology (pO2 = 37 mmHg with FiO2 0.21). The patient did not require oxygen support before introduction to anaesthesia.
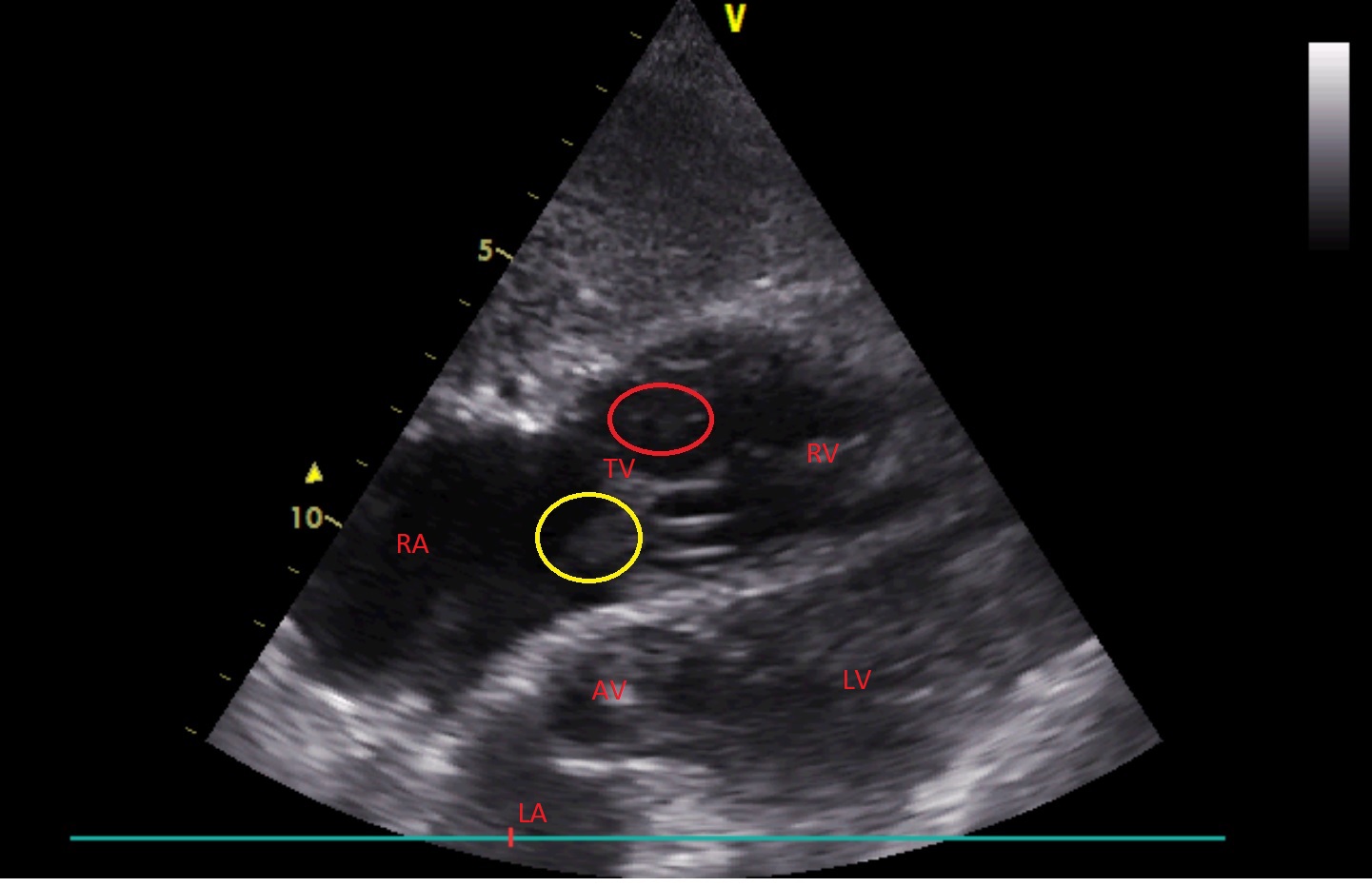
Ultrasonography was performed to reveal the cause of hypoxemia. We started with lung ultrasonography:
<h3>
