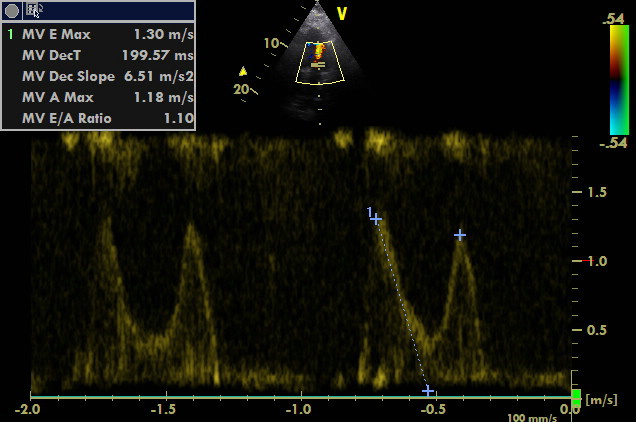
An older woman was admitted to the ICU for hypotension and renal failure.
During admission: blood pressure 80/40 mm Hg, heart rate by 80 bpm, no oedema, slight dyspnea, BMI 35. Lab tests showed no signs of infection, creatinine level was very high of 750 umol/l (8.5 mg/dl), urea 30 mmol/l (85 mg/dl), K+ 5.7 (mmol/l), mild metabolic acidosis well-compensated by respiration. Anuria.
A history of hypertension, chronic ischemic heart disease and nephrectomy on the right side. Antihypertensive therapy was adjusted 14 days ago because of decompensation (direct and indirect vasodilators, including ACEI). At that time, creatinine was 200 umol/l (2.26 mg/dl).
The question is why the patient presents with hypotension? Differential diagnosis encompasses hypovolemia, cardiogenic aetiology, vasodilation caused by medication and infection (which is not probable when considering results of lab tests).
We performed POCUS: