A 64-year-old patient with a history of hypertension and chronic ischemic heart disease (coronarography without the necessity of intervention two years ago) taking sartan has suffered from respiratory infection for the past two weeks, without antibiotic therapy. Her health condition worsened two days ago, when dyspnea, pain in the right hemithorax propagating to the right side of the neck with relation to respiration and non-productive cough appeared. She did not measure her body temperature at home. She comes to the emergency departement.
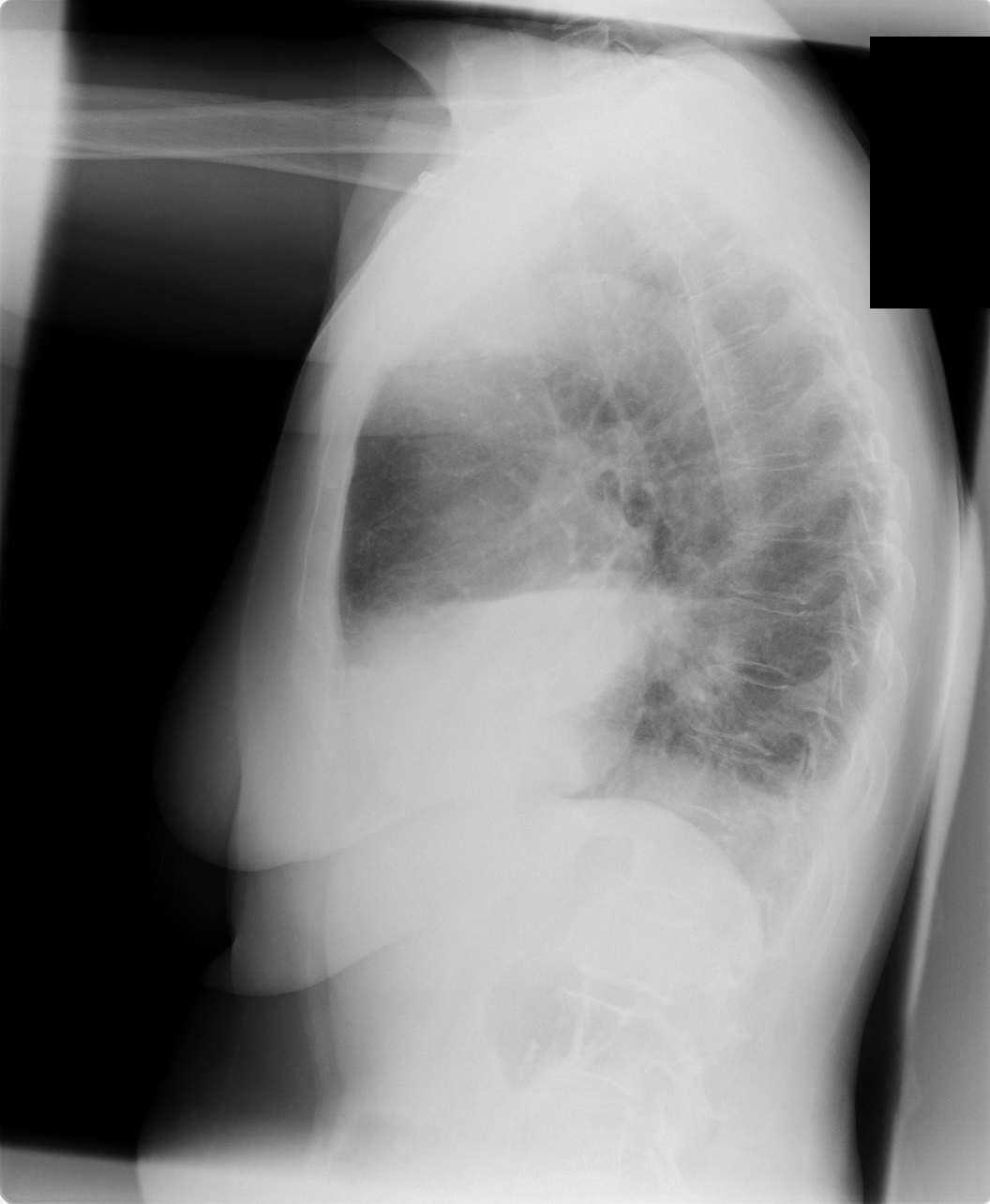
She presents with fever 38.6 °C, lab tests, including blood cultures, were taken and chest X-ray was performed – see the image below. The auscultation revealed crackles and silent breath sound dorsolaterally on the right side. Respiration mechanics was normal by respiration rate of16/min. SpO2 90% with nasal cannula 3 l/min. Hemodynamics was stable, neck and abdomen without a pathological finding. Lower limbs without oedema.
Her chest X-ray:
Differential diagnosis encompasses pleural effusion or infiltration on the right side.
Lab results: CRP 385 mg/l, leukocytosis 35000 with 92 % of neutrophils, procalcitonin 11 ng/ml. Lactate, base excess as well as other values were normal.
Head of the department recommended contrast CT scan of chest and abdomen and consultation with ICU for eventual admission (as sepsis).
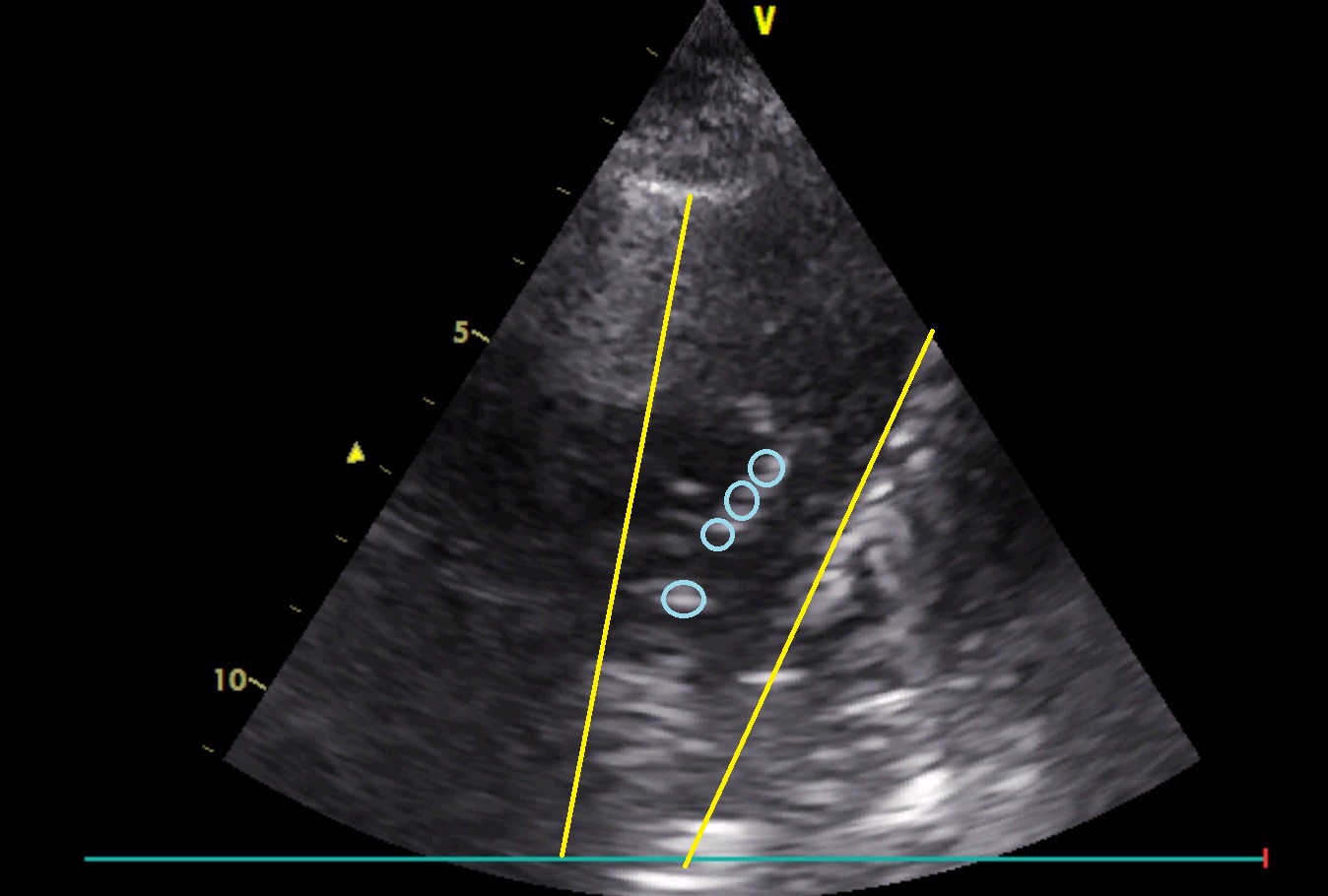
Bed-side ultrasonography of the right hemithorax was performed before the CT scan (the patient was in the upright position):